When is “co-morbidity” no longer “co-morbidity”?
When is “co-morbidity” no longer “co-morbidity”?
The conceptual wall between ASD as a “developmental disorder” versus anxiety, depression, mood disorder and schizophrenia as “psychiatric disorders” or “mental illness” needs to come down. Indeed, within the scientific community, it has already come down: ASD, ADHD, anxiety disorder, bipolar disorder, and schizophrenia share common genetic roots, co-migrate within families, and co-occur within individuals – either simultaneously, or sequentially (that is, some individuals start out with clinical features of ASD, and wind up with clinical features of anxiety disorder, depression, mood disorder, or schizophrenia).
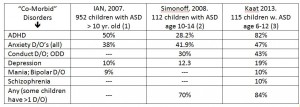
Unfortunately, we are held prisoners by old ideas and outdated terminology. In the present instance, the term “co-morbidity” conveys the message that anxiety disorder, depression, mood disorder, ADHD, and even schizophrenia are present in addition to an individual’s ASD, rather than as integral elements of the person’s neurobehavioral disorder. Here I have summarized three studies that illustrate what I’m talking about. Each study used slightly different methods and obtained somewhat different results, but the overall pattern is clear:
When you purchase a car, you may have options: Sunroof? Power steering? Trim package?
Different buyers order different options. But once they are installed, you no longer think of them as existing “in addition to” the car; you think of them as “part of” the car. It’s the same thing with ASD and the various “mental health disorders.” Combinations vary from one person to the next (As the expression says: “When you’ve met one person with ASD, you’ve met one person with ASD.”) But when the rate of co-occurrence of these “mental health disorders” approaches 100 percent, they cease to be “co-morbidities.” Rather, they become part of the base package.
(1) IAN Research Report #1 – May 2007; http://www.iancommunity.org/cs/ian_research_reports
(2) Simonoff, E., et al., Psychiatric Disorders in Children with Autism Spectrum Disorders: Prevalence, Comorbidity, and Associated Factors in a Population-Derived Sample. Journal of the American Academy of Child & Adolescent Psychiatry, 2008. 47(8): p. 921-929
(3) Kaat, A.J., K.D. Gadow, and L. Lecavalier, Psychiatric Symptom Impairment in Children with Autism Spectrum Disorders. Journal of Abnormal Child Psychology, 2013
James Coplan, MD is an Internationally recognized clinician, author, and public speaker in the fields of early child development, early language development and autistic spectrum disorders.















Leave a Reply